From diagnosis to discharge, surgical care involves several key teams. While these teams are fundamentally interconnected, they often function in relative isolation, focusing on their specific responsibilities before passing the baton to the next group. This blog explores how this dynamic both reflects and perpetuates the creation of silos, and how these silos can affect the quality and efficiency of perioperative care. We’ll also share strategies to help break down barriers, foster collaboration, and leverage our collective strengths to achieve the highest standards.

### Beyond Business Jargon
Silos might sound like a buzzword, but they're everywhere—so much so that they made Forbes' list of the most annoying business jargon at number 20. Discussions about “breaking down silos†have become a staple in boardrooms and workshops, causing dread among those hoping to wrap things up quickly.
This phrase's popularity stems partly from its universality. Many of us have witnessed issues caused by poor communication between departments. Think of surgical technicians not communicating with sterile processing staff, anesthesiologists not talking to recovery teams, or surgeons operating in isolation. Over time, these behaviors prioritize the goals of individual teams over the organization as a whole, leading to inefficiencies that compound over time. Silos emerge naturally from these dynamics.
Gillian Tett, in her book *The Silo Effect*, provides a broader perspective on this phenomenon. She argues that silos represent a systemic fragmentation within organizations, where different units operate independently, essentially leaving the right hand unaware of what the left is doing. Her critique draws parallels with the structures of large investment banks, where internal divisions act as competing tribes with their own objectives, language, incentives, and cultures. Familiar, right?

### Breaking Free from Bias
Tett also highlights the mental silos individuals construct based on their backgrounds and cultural experiences, which lead to tunnel vision. People tend to focus on what they already know, surrounding themselves with like-minded colleagues and reinforcing existing ideas. This mindset perpetuates repetitive mistakes and missed opportunities for growth.
Both structural and individual silos are prevalent in surgery. Our work is organized around specific teams and tasks, shaped by traditional hospital hierarchies and training programs. These divisions foster strong tribal identities and habitual behaviors, creating silos that, though flawed, serve practical purposes. As Tett notes, “The modern world needs silos; humans need to create structure to manage complexity.â€
Rather than simply dismantling silos, we should aim to master them by overcoming the silo mentality—characterized by inward focus, resistance to sharing, and reluctance to adapt. Stepping beyond our biases allows us to critically assess our processes, collaborate effectively, and enhance outcomes.
> “The challenge is not to rid ourselves of silos but to master them, instead of allowing them to master us.â€
>
> —Gillian Tett, *The Silo Effect*
### High-Risk Silos in Surgery
Identifying silos in surgery is relatively straightforward, especially given the traditional, hierarchical structure of most hospitals. Exceptions exist, such as the Cleveland Clinic under CEO Toby Cosgrove, which pioneered innovative approaches to organizational design.
These silos manifest across the perioperative continuum, as illustrated in the patient journey timeline (Fig 1). Each phase includes sub-stages tied to specific locations and teams responsible for delivering care. The intraoperative period, highlighted in green in Fig 1, is particularly complex due to its reliance on the operating room (OR) and significant resource allocation.

During surgery, multiple teams and workflows converge, creating a highly intricate and safety-sensitive environment. Often, processes occur simultaneously, with one team preparing for the next step while another focuses on the current task. Studies show that this complexity heightens risks, making it prone to errors, information loss, and miscommunication—all hallmarks of a silo mentality.
### Bridging Team Boundaries
Poor communication between groups is a defining feature of silos. In fields like aviation, nuclear power, and healthcare, communication breakdowns are a leading cause of adverse events. Researchers in the OR found communication failures in 30% of team exchanges, with one-third posing patient safety risks. In Washington, communication failures contributed to injury in 43% of perioperative anesthesia malpractice claims, mostly occurring during the intraoperative phase.
Beyond direct harm, silos create inefficiencies. Observations in Chicago revealed 67 communication failures in the OR, with 36% related to equipment and 24% linked to insufficient updates about procedure progress. These lapses often result in delays and wasted resources.
A 2017 systematic review examining process mapping in the OR identified common inefficiencies at points where team workflows intersect, such as patient transfer, instrument setup, and anesthetic handovers.
> “Communication failures frequently occur when the siloed workflows of two or more teams fail to interface as planned.â€
### A Common Language for Surgery
How can we address silos in surgery? One solution lies in data sharing. Data silos, which isolate information within a single unit, often lead to inconsistencies and redundancies. Initiatives like Integrated Care Pathways, Enhanced Recovery After Surgery, and the Perioperative Surgical Home have demonstrated the benefits of open data access, improving outcomes and efficiency through shared resources.
At Incision, we’ve developed a universal surgical language to standardize and communicate procedures. This framework, supported by an online academy offering over 750 courses filmed live in the OR, has reduced errors and enhanced performance. Accredited by the Royal College of Surgeons of England, the academy boasts over 170,000 users globally.

### Connecting Teams Digitally
Facilitating cross-team communication on the work floor is challenging without digital tools. Mobile technology is now revolutionizing this aspect.
Incision Assist, a mobile app, connects interdisciplinary teams with unit-, team-, and surgeon-specific resources and protocols. It improves information access, increases familiarity with equipment, and streamlines cross-team processes like patient turnover.
Imagine this scenario: In the holding bay, the pre-op team uses Assist to confirm anesthesia readiness, including the video-guided system preferred by this anesthesiologist. Meanwhile, the OR is prepared exactly as this surgeon prefers, eliminating equipment confusion. The surgery begins on time.
Midway through, recovery checks the app for details about drain placement. Post-op instructions are clear: no antibiotics, food after four hours, discharge to the ward, follow-up review tomorrow. Protocols are accessible, up-to-date, and tailored to each team.
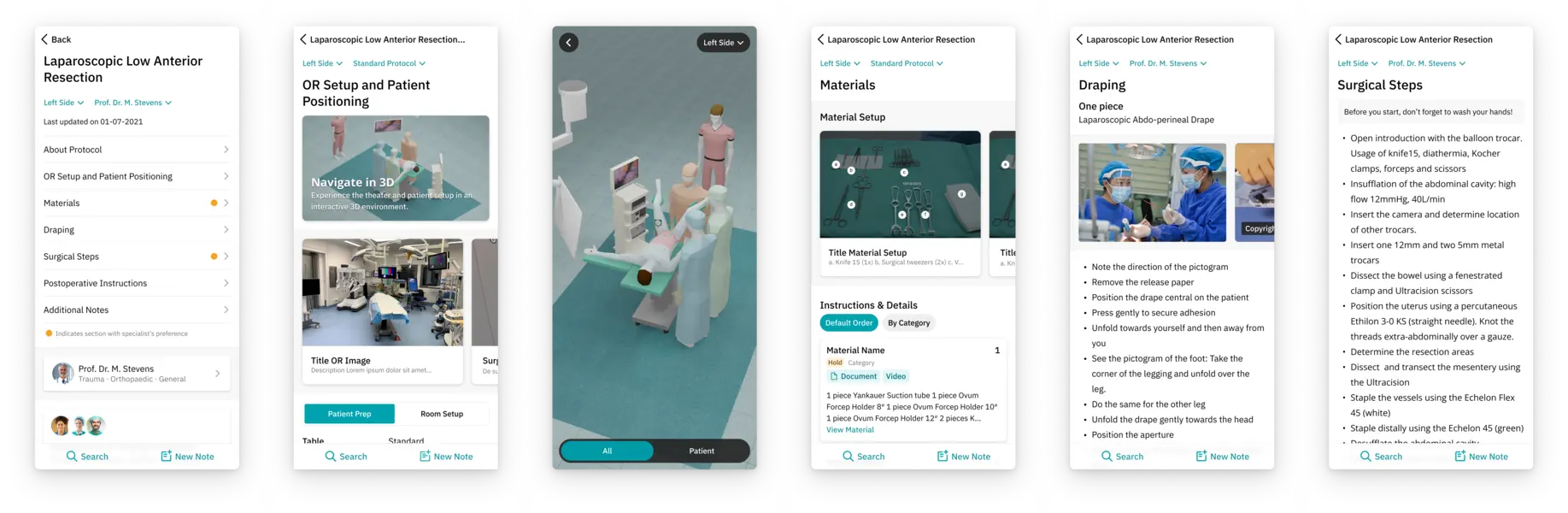
By connecting our silos rather than dismantling them, technology empowers us to leverage our collective strengths. At Incision, we’re committed to fostering conversations that unite teams, educate dynamically, and inspire growth. Join the dialogue!
Follow us on [LinkedIn](#), [Twitter](#), or [Facebook](#).
---
This updated version maintains the original message while refining language and structure for clarity and engagement.
HbA1c And Blood Glucose Test Quality Control
A1Cchek Pro, A1Cchek Express, HbA1c Quality Control Reagent, Glycohemoglobin Quality Control
Wuxi BioHermes Bio & Medical Technology Co., Ltd. , https://www.biohermesglobal.com